Bladder and Urethral Slings
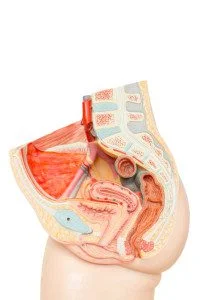
Bladder and urethral sling surgeries are used to treat urinary incontinence that cannot be successfully treated with medication. A surgeon uses your own tissue, strips of synthetic mesh, or animal or donor tissue to create a sling under your urethra or bladder neck. The sling supports the urethra and helps keep it closed to prevent urine leakage.
Types of Sling Procedures
- Tension-free sling. No stitches are used to attach a tension-free sling. Instead, body tissue holds the sling (which is made from a strip of synthetic mesh tape) in place. Scar tissue eventually forms around the mesh and keeps it from moving.
There are three approaches to a tension-free sling procedure:
-
- Retropubic. A surgeon makes a small incision inside the vagina and two small openings above the pubic bone just big enough for a needle to pass through.
- Transobturator. A surgeon makes an incision similarly in the vagina, but also creates a small opening on each side of the labia for a needle to pass through.
- Single-incision mini. A surgeon has only one small incision in the vagina to perform the procedure.
- Conventional sling. A surgeon makes an incision in the vagina and places a sling made from synthetic mesh tape, your own tissue, or tissue from an animal or deceased donor under the neck of the bladder. The sling is pulled through another incision in the abdomen to adjust tension. Each end of the sling is then attached to the fascia (pelvic tissue) of the abdominal wall using stitches. This type of surgery can require a larger incision than a tension-sling.
Who is a good candidate for sling surgery?
The typical patient has moderate to severe urinary incontinence where the cause of the problem is known and the problem has not been alleviated by less invasive options such as medications and physical therapy.
Bladder Fistula
A bladder fistula is an abnormal connection between the bladder and another organ or skin. The most common forms of bladder fistulas involve:
- The bowel (enterovesical fistula)
- The vagina (vesiovaginal fistula)
Although relatively rare, fistulization to the skin can result from an injury or previous surgery in the face of bladder outlet obstruction.
The biggest issue with fistulas is that they are created by infection, and they carry this infection to any organ they connect to. For example, if it tunnels out and connects to the bladder, a bladder infection can devlop.
Who is at risk for developing a bladder fistula?
- The most common reason for a bladder fistula is an inflammatory bowel disease, such as Crohn’s Disease or diverticulitis. Around 25% of people with Crohn’s Disease will develop a fistula.
- Approximately 20% of bowel fistulas are caused by bowel cancer.
- Fistulas may also develop as a result of previous radiation therapy.
Causes
Inflammation
- Inflammation of the lining of the digestive tract causes the intestines to form scar tissue and become abnormally thick.
- This thickening can lead to the formation of ulcers on the inside lining of the intestines.
- When the ulcers grow deeper, they can begin to burrow through the wall of the intestine, forming a tunnel that leads to whatever tissue is next to the sore.
Abscesses
Anal abscesses are often linked with fistulas and result from an infection of the small glands inside the anus. Crohn’s disease increases the risk of infection of these glands.
Symptoms
Common symptoms of bladder fistula include:
- Frequent urinary tract infections
- Passage of gas from the urethra during urination
- Urinary leakage
Diagnosis
A doctor may administer the following tests to diagnose a bladder fistula:
- Excretory urogram.- an x-ray examination of the bladder in which contrast dye is injected into the patient’s system and its progress through the urinary tract is recorded to study the anatomy and function of the bladder and urinary tract.
- CT Scan
- Cystogram (bladder x-ray)
Recovery From a Bladder or Urethral Sling
After surgery, you may feel weak and tired for several days. Your pubic bone may feel bruised, and you may have some pain or cramping in your lower belly. These symptoms should get better in 1 to 2 weeks. You also may have some vaginal spotting for up to 1 month. This is normal.
You should have less or no urine leakage when you sneeze, cough, laugh, or exercise. In fact, at first, you may find that it is harder than usual to empty your bladder. This usually gets better after 1 or 2 weeks.
You will probably be able to go back to work in 1 to 2 weeks. But you will need at least 6 weeks to fully recover before returning to all normal activities. You must avoid heavy lifting and strenuous activities during this time. These might put extra pressure on your bladder while you recover.
Sexual Function
If you are receiving a bladder or urethral sling you can expect to not be doing sexual activity for some time. Your body will need to recover from the surgery and get used to having the sling. Over time, however, your sexual function should not be impacted by receiving a bladder or urethral sling. If you are having new or worsening sexual function after surgery make sure to contact your doctor to discuss!